
Definition
Fractures of the proximal humerus involve a break of the large upper portion of the arm bone close to the shoulder joint.

Pathology
Proximal humerus fractures are the most common type of fractures following those to the hip and the distal radius (small bone of the forearm). They result from direct trauma to the upper arm and shoulder or by axial loading through the lower arm. Stress fractures can occur with overhead throwing (cricket and baseball players) or with violent muscle contractions (seizures). They are almost exclusively closed fractures. Open fractures are accompanied with severe soft tissue injuries increasing the risk of infection. Often concomitant with proximal humerus fracture, the integrity of the rotator cuff is compromised requiring surgical repair. High-energy fractures of the proximal humerus can be associated with vascular injury especially when located near the head. Nerve injury, more frequently to the axillary nerve may result in temporary paralysis and only seldom in permanent damage (8%). With severe chest trauma the patient may present pneumothorax or lung collapse that severely affects the respiratory function.
Classification
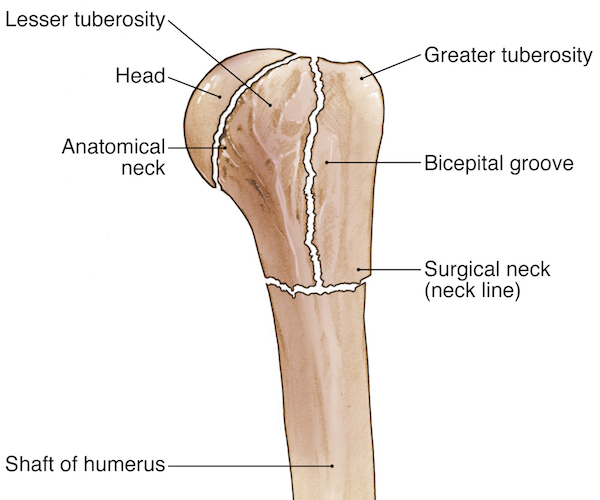
The Neer classification is used to distinguish amongst different proximal humerus fractures and relies on the anatomical location of the fracture, which includes one or more of the following parts:
Articulating surface
Greater tuberosity
Lesser tuberosity
Humeral shaft
The fracture is defined as displaced when one of the four elements is separated by over 1 cm or is angulated by more than 45°.

The fractures to the proximal humerus are divided into:
Type 0 one fractured part without dislocation
Type A two-part fracture of the great tuberosity and lesser tuberosity avulsion
Type B involves the humerus “surgical” neck below the femoral head as two-part, three-part and four-part with one or both tuberosities
Type C involves the humerus anatomical neck (between the head and greater tuberosity) as two-part, three-part and four-part with one or both the greater and lesser tuberosities

These are defined further as:
One-part fractures are non-displaced fractures or fractures with minimal displacement
Two-part fractures only involve a single segment
Three-part fractures involve two segments
Four-part fractures occur when all humeral segments are involved (see image in pathology section)
The injury severity is proportional to the increasing number of fractures.

Causes
Proximal humerus fractures occur through a range of mechanisms such as a direct blow to the shoulder, a fall to the side, a fall on the outstretched arm and an impact during motor vehicle accidents. Such fractures are often observed in the elderly after a fall from standing, or while walking on flat pavement or stairs and it is the third most common type of fracture in this age group. Pathologic fractures of the humerus may ensue with minimal trauma when patients suffer from conditions that weaken the bone. In young individuals a proximal humerus fracture is the result of high-energy trauma caused by motor vehicle accidents and sport injuries. While proximal humerus fractures are predominant in older females, in the young populations they are more frequent in males.

Risk factors
Frequent risk factors for a proximal humerus fracture include elderly age, chronic medical conditions that reduce bone density as well as life-style and physical activities exposing to possible traumatic injuries.Additional risk factors are:
Osteoporosis
Muscle weakness
Vision impairment
Seizure
Low blood pressure
Professions involving extensive driving
Sports (riding, cycling, skiing, snowboarding)Diabetes mellitus
Paget's Disease
Bone cyst

Symptoms
The clinical symptoms of a fracture to the proximal humerus are quite evident and include:
Sharp, intense pain of the shoulder/upper arm at the time of accident, increasing with movement
Severe swelling
Tenderness over the shoulder and upper arm
Presence of bruises extending below the fractured area, chest and arm Inability to move the arm
Lost sensation over the deltoid muscle (axillary nerve injury)
.jpeg)
Diagnosis
The medical history of the patient will determine the mechanisms and type of injuries sustained. Clinical examination will assess the presence of swelling, tenderness at touch, inability to move the arm and involvement of additional injuries (glenohumeral dislocation, clavicle fracture, nerve injury) and damage to the axillary nerve.A fracture to the proximal humerus is generally confirmed by X-rays of the shoulder taken under the antero-posterior, lateral and scapular views.

A CT scan is useful in preparation for surgery to evaluate the type of fracture and the presence of bone fragments within the joint. MRI is employed less frequently when damage to the rotator cuff or other soft tissues is suspected.
Treatment

Nonoperative treatment
The treatment modalities for a proximal humerus fracture largely depend on the condition of the bone, as well as the age and physical state of the patient. Conservative treatment is successful in about 75% to 85% of cases if the fracture is stable and is not displaced. It consists in the use of a cast or sling named shoulder immobiliser with the arm hanging at 90 degrees to place traction to the fractured bone. Traction is recommended to align the fragments if a mild displacement is present. Administration of anti-inflammatory medications (NSAID) assists in reducing inflammation and swelling while analgesics are given to reduce pain. Fracture healing and bone union take approximately 6-8 weeks.

Surgical treatment
When major displacement of the fractured bone parts occurs or in case of open fractures, surgery is required. Surgical treatment can be achieved through a variety of techniques:
Closed reduction with percutaneous fixation using screws inserted through the skin
Open reduction with internal fixation (ORIF) is indicated with a displaced fracture to hold bone fragments together using metal plates and screws, rods, wires
Intramedullary nailing consists in the insertion of a metal rod through the humerus cavity where the marrow is located
External fixation involves is employed when immediate surgery is not possible with a frame applied over the shoulder fixed with percutaneous pins. This is followed by ORIF at a later stage.

Prosthetic replacement of the fractured bone(s) via:
Hemiarthroplasty consists of the replacement of the entire humeral head using a ball with a stem inserted in the humerus cavity or a partial replacement of the humeral head following the resurfacing of the bone
Total shoulder replacement includes substituting both the humeral head and the glenoid or shoulder socket maintaining the bones relationship.
Reversed total shoulder arthroplasty is similar to the previous whereby the prosthetic elements are reversed and glenoid becomes the humeral head and vice versa (see figure with different examples)
Open fractures require antibiotic therapy. Union of the proximal humerus fracture takes over 8 weeks or longer if complicating factors arise. Outcome following proximal humerus fracture much depends on the type of fracture sustained with a four-part fracture and the elderly age of the patient often resulting in limited functional recovery. It is expected that a year is required for full recovery.

Rehabilitation
In case of conservative treatment of a stable proximal humerus fracture physiotherapy can begin after one week by performing gentle shoulder rotation exercises with more energetic physiotherapy after 3 weeks or after the bone has completely healed. Following surgery a sling is used for a few days up to six weeks to immobilise the arm until gentle full physiotherapy treatment can begin. Early rehabilitation consists in oscillating the suspended arm to minimise the force as shown in figure. This is followed by active and passive exercises to strengthen the shoulder muscles and restore function. A number of exercises are available to strengthen the musculature of the shoulder and shoulder blades.
Physical therapy can last two to four months. It is recommended for athletes to return to sport not prior to three months after surgery. In the rehabilitation phase applications of cold pads, administration of painkillers and anti-inflammatory therapy with NSAIDs can assist in managing the symptoms. Physiotherapy also includes:
Massage and joint manipulation
Joint mobilisation
Ice/heat treatment
Physical exercise (pendular movements, shoulder shrug, rotation)
Isometric strengthening followed by active strengthening of the rotator cuff muscles
Education in sport and daily activities for overhead movements
Return to sport plan
Complications
A fracture to the proximal humerus may result in a number of complications whether conservative or surgical treatment has been employed. Below is a list of the most common complications:
Adhesive Capsulitis or frozen shoulder: common pathology preventable with physiotherapy
Non-Union: when the two bone extremities fail to heal and unite
Mal-Union: when the fracture heals with an altered position resulting in movement impairment
Avascular necrosis: partial death of the humeral head when blood perfusion to the bone is compromised. This is mostly ensuing in 2 and 4-part fractures
Arthritis: of the shoulder joint is along-term complication caused by altered shoulder joint structure and movement
Stiffness: of these shoulder joint
Nerve injury: usually resolves spontaneously but can take months

Prevention
The main preventative strategy for a proximal humerus fracture and its associated complications is to avoid falls, high energy impacts and improve bone density. Particularly in the elderly the following measures are recommended:
Osteoporosis treatment
Calcium supplement intake
Regular exercise
Use of a walker if balance is poor
Use of handrails when walking on stairs
Wear shoes with rubber soles
Remove any hazards at home that increase the risk of falls
Shoulder taping is useful to stabilise the shoulder when returning to sport practice